Atopic dermatitis in infants
This post was written by Dr. Pleimes, a specialist in pediatrics, dermatology and allergology
Click here to read further information about Dr. Pleimes.
Basics, causes & affected body parts
What does neurodermatitis / atopic dermatitis / atopic eczema mean?
- Neurodermatitis is medically synonymous with the terms atopic dermatitis, atopic eczema or endogenous eczema.
- Dermatitis/…dermitis is an inflammation of the skin.
- Atopy refers to the increased tendency of the immune system to become involved with otherwise harmless environmental substances (allergens) and to react to these for no reason.
- Neuro… (from Greek neuron = nerve) is actually an outdated and also no longer correct designation, which, however, remains anchored in everyday language use. It used to be thought that neurodermatitis was caused by a nerve disease, but this is now disproved.
The inflammation (dermatitis) on the skin manifests itself as so-called eczema:
Eczema describes: reddened skin with scaling and rough skin surface and accompanying usually itching. Eczema occurs frequently, especially in the first years of life. The cause is a not yet fully developed protective function of the skin. Many people also have a family history of sensitive skin and/or an easily irritated immune system. This is not a disease in itself, but leads to the fact that environment and environmental factors (sweat, saliva, bacteria, food, soaps, friction, etc.) irritate us more easily. It also causes moisture to be lost from the skin more quickly, resulting in dry even more sensitive skin. Those who repeatedly get eczema, i.e. skin inflammation, with this innate sensitivity then have atopic dermatitis or neurodermatitis.
Good news: if the skin becomes more stable with increasing age, the problem can also “grow out”. However, the inherited sensitivity remains for the rest of the patient’s life.
In infants, skin symptoms of atopic eczema usually do not manifest themselves until after the 3rd month of life. Before this time, however, other inflammations of the skin can occur, which are skin diseases independent of atopic dermatitis:
In the first 2 months of life, an increased sebum production is often still found and here baby acne or often more localized in the diaper area or the skin folds seborrheic eczema are more common. These two skin diseases, although they can be very pronounced in individual children, are harmless and usually disappear by themselves within a short time. We often see transitions or mixed pictures of e.g. seborrheic eczema and atopic eczema in the first half of life, which is especially important for the correct treatment of the skin. While the initial skin problems such as baby acne or seborrheic dermatitis should have little fat in the care, later the sensitive skin in atopic dermatitis usually benefits from richer products.
What is the cause of atopic dermatitis?
Our epidermis is not yet fully mature after birth, but still shows increased permeability. It becomes much more stable, especially in the first 2-3 years of life. Especially in the first months of life, but also afterwards, there is therefore increased contact of the immune system (active in the deeper layers of the skin) with irritating substances in the environment (bacteria, dust, mites, pollen, saliva, sweat, food, etc.). The recurring irritation can then cause inflammation (a thickening, reddening, scaling of the skin, i.e. eczema). The messenger substances released in this process are not only involved in the change of the epidermis, but also irritate itch fibers and inhibit certain defense functions of the skin. The skin becomes unbalanced.
If the skin stability is measured at the affected eczema sites, it is unfortunately even worse there than at previously only sensitive “healthy / unaffected” skin. This ends in a vicious circle (sensitive skin – irritation – inflammation – more sensitive skin…), as further inflammation is now intensified, especially at existing eczema sites.
Which areas of the skin are particularly affected?
In infancy, eczema of the cheeks / atopic dermatitis of the face often occurs initially. On the body, especially the abdomen and chest area are affected and on the arms and legs usually even more the extensor sides. Eczema can also exist on the hairy head. The diaper area, on the other hand, is typically left out or only very slightly affected.

If there is a tendency to sensitive and dry skin, especially if a child’s parents have or have had hay fever, allergies, asthma or even eczema, early basic skin therapy is important.
This includes 2 measures:
- The careful removal of trigger factors (irritating factors) through regular but very gentle skin cleansing (syndets / bath oils).
- A skin protection therapy after the bath or shower. For this purpose, creams (i.e. mixtures of water and fat) are spread on the skin of the entire body.
Basic rule: the drier and less acutely reddened the skin, the more fat. But never pure fat or oil without water content as care, this would not improve dry skin.
For weeping highly red, acute areas, little or no fat is used for a short time. Here, for example, a few days of black tea compresses can be helpful.
If lighter spots heal under basic therapy, everything is fine. Often, however, the skin is so badly damaged by the existing inflammation that we cannot rebalance the skin barrier with protection alone. In addition, itching caused by scratching and rubbing can always cause further damage to the skin. Our strongest opponent here is the existing inflammation. If we manage to stop it completely, the skin can rebuild itself to its current possible best state. This state is then easier to keep stable.
Anti-inflammatory therapy for atopic dermatitis
 Important: What should the therapy achieve?
Important: What should the therapy achieve?
The goal is always to achieve a completely eczema-free child at an early stage. This condition should be maintained as long as possible.
There are 2 groups of substances with good efficacy against inflammation
- On the one hand the group of cortisone preparations
- On the other hand the calcineurin inhibitors
Both have their advantages and disadvantages and when used correctly (unfortunately contrary to general perception) are extremely safe preparations with few side effects. This is true even when used on infants.
In order to avoid side effects, however, you need the information: how long, on which area, which preparation should be applied. A good atopic dermatitis therapy always includes an individual treatment plan that specifies when, what and how the skin should be treated.
Face, diaper area and maintenance therapy are often areas of application for calcineurin inhibitors. On the rest of the body, modern cortisone preparations with a very good safety profile can be used.
Shouldn’t I wait until my child is a little older? Then perhaps the preparation will be better tolerated?
The earlier a treatment is carried out, the shorter the treatment usually has to be. The lower the risk of inflammation becoming chronic.
Encouragingly, cortisone creams and approved alternatives can also be used well in very young infants. However, the right choice of preparation should be made by a specialist with experience.
Shouldn’t I wait until my child is a little older? Then perhaps the preparation will be better tolerated?
The earlier a treatment is carried out, the shorter the treatment usually has to be. The lower the risk of inflammation becoming chronic.
Encouragingly, cortisone creams and approved alternatives can also be used well in very young infants. However, the right choice of preparation should be made by a specialist with experience.
Won’t the eczema come back immediately if I stop treating it?
Especially in the first years of life, there is an increased risk of eczema due to the still very sensitive skin barrier. Sometimes only ONE additional factor is enough to trigger a new flare-up. And, YES, this one should be treated again. As your child gets older, non-inflamed skin becomes more stable and the likelihood of new inflammatory episodes decreases.
What are the side effects of cortisone therapy?
With cortisone, it is important to always have breaks between treatments of a particular area of the skin. However, in the initial phase, with the right preparation, it is quite possible to treat a few weeks a little more intensively and then with a maintenance therapy a little more, without expecting any problems. The risk of side effects exists if one and the same area always has to be treated and no breaks can be built into the therapy. If other areas of the skin are repeatedly affected and treated, regular application is also unproblematic.
How can I prevent new eczema from developing again and again? Do I then have to regularly apply therapy creams again and again?
The stronger and longer eczema has existed, the longer the skin needs to regain its natural, stable balance. After an eczema has healed, we do not stop further treatment completely, but still carry out a pro-active (preventive) maintenance therapy. The goal here is to maintain a completely eczema-free skin, i.e. we apply the therapy creams to skin that now looks healthy to you. However, this therapy is no longer carried out daily, but only e.g. 2 days per week.
Fat-moist dressings
For the somewhat larger children, intensified basic therapy measures are usually suitable, e.g. for persistent eczema on the arms or legs. For this, care, or sometimes therapy creams (only on medical instruction), can be applied under a bandage. A moist bandage over a very greasy care cream (over it again a dry bandage) strengthen the deep effectiveness of the care products.
Atopic dermatitis pajamas
For generalized eczema, additional textiles can be helpful, as their smooth surface and coating help reduce itching and scratching, as well as bacteria on the skin.
If we just keep treating, how do I find out the cause of the eczema / atopic dermatitis / skin inflammation?
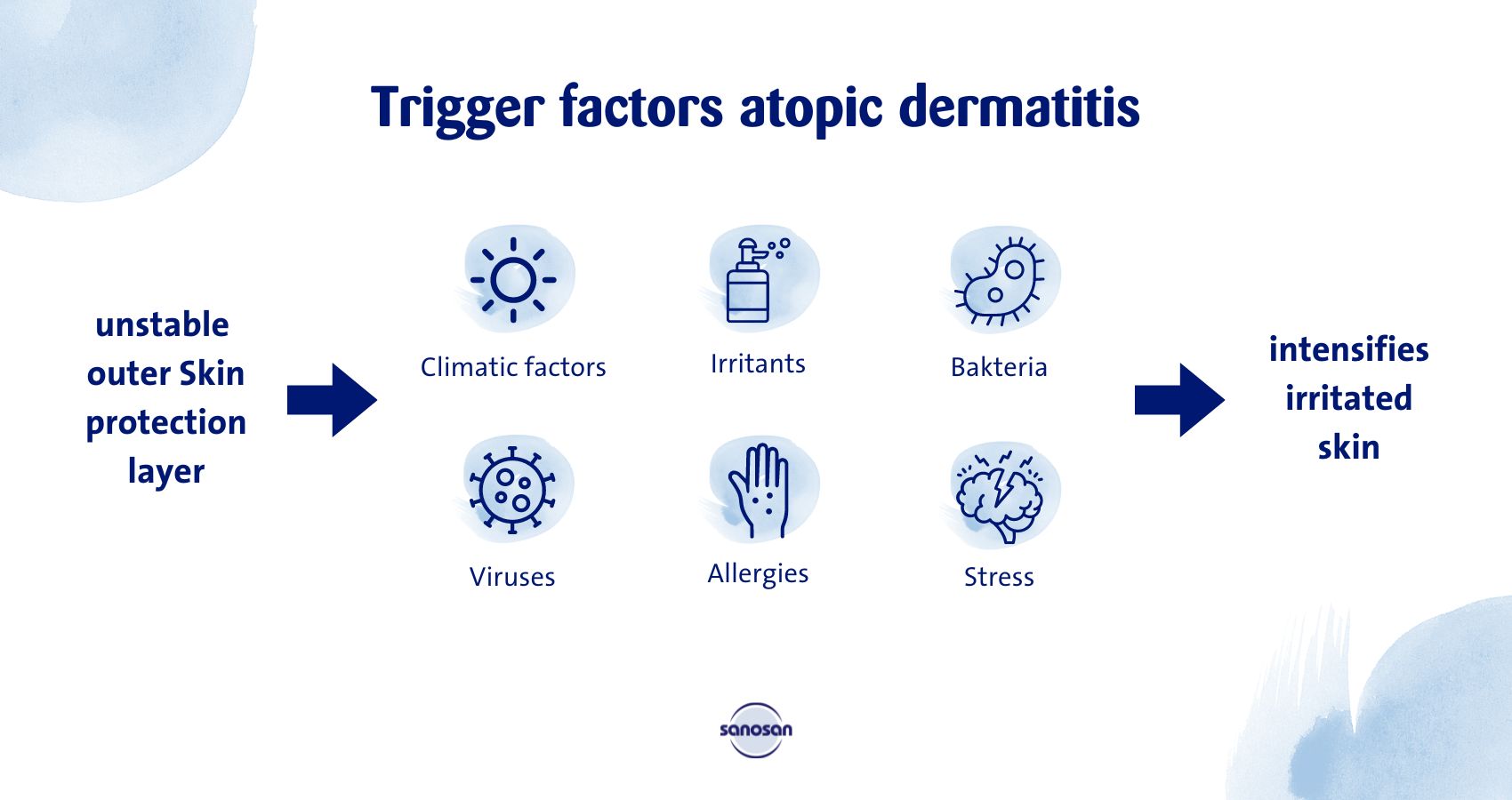
The cause is known: The outer protective skin layer is not yet as stable as it could be optimally. And sometimes the immune system reacts faster to stimuli than it should. This leads to various factors (trigger factors see below) in the environment irritating us. And if the inflammatory system is already slightly active, everything that irritates us from “inside” can also worsen the situation (e.g. infections, vaccinations, teething, stress).
Trigger factors: Factors that can trigger relapses but are not the cause of the disease.
- Climatic factors: Drying of the skin, heat (increased itching), sweating
- Irritants: soaps, wool clothing, acids in food, etc.
- Bacteria: e.g. staphylococci, streptococci, yeast fungi
- Viruses: e.g., herpes viruses, pox viruses (dell warts)
- Allergies: Food, dust mites, pollen, etc.
- Stress: intensification of itching
Allergies
With a sensitive outer protective layer of the body, contact with environmental allergens (food or pollen / house dust) is increased. Together with an immune system that is more easily irritated, this also increases the risk of developing additional allergies.
Allergy means that our defense system perceives an actually harmless substance as dangerous and stores a defense against it. This can lead to acute allergic reactions such as hives or tightness of the respiratory tract, but also only to a worsening of eczema. Fortunately, allergies that directly worsen eczema exist but only in a small proportion of children.
When should an allergy test be done?
We test for allergies when a constant eczema condition persists (e.g. more than 4-8 weeks) despite all the above measures. Also in case of very pronounced, severe eczema or definite indications in the medical history, a test may be useful. In this case, a blood sample of the child is usually examined.
Vaccinations
There is no evidence to justify skipping vaccinations in children with atopic dermatitis. In fact, children with severe atopic dermatitis should be vaccinated against diseases such as chickenpox at an especially early age because of the increased risk of increased scarring and bacterial skin and soft tissue infections due to the impaired skin barrier.







Comments (0)